August 13, 2024 • 7 Min Read
In today’s dynamic healthcare landscape, hospitals, health systems and medical groups face formidable challenges and opportunities. The sustainability of these entities hinges on their ability to confront and mitigate pervasive issues such as nurses' and physicians' burnout while ushering in transformative changes to care and operating models through innovative business approaches and technology integration.
Digital health and care delivery are transforming how patients access care and how and where they experience it. With new entrants seizing digital opportunities, traditional healthcare organizations must further advance their efforts to compete in this new ecosystem.
Healthcare organizations should embark on a journey of fundamental reimagining, exploring novel approaches to care delivery and administration.
Recognizing the urgency of the situation, healthcare organizations should embark on a journey of fundamental reimagining, exploring novel approaches to care delivery and administration that align with the evolving demands and complexities of the healthcare landscape.
This article delves into the pivotal trends shaping healthcare provider strategies, highlighting the imperative shifts required for navigating the unprecedented challenges and opportunities that lie ahead.
Seizing Synergies: Navigating the Evolving Landscape in Mergers and Acquisitions
The current economic environment indicates a heightened probability of industry consolidation, particularly evident in the evolving M&A dynamics involving payers, providers and life sciences organizations. This shift signifies a strategic move towards prioritizing value creation for patients and ensuring sustainability. The current healthcare landscape revolves around effectively navigating the evolving M&A landscape, impacting various stakeholders, including payers, providers and leaders in life sciences.
Creative payer-provider arrangements, or ‘payvider’ models, will continue to evolve to provide more integrated and coordinated care.
The ongoing consolidation trend, observed in the growth of larger integrated delivery systems both nationally and locally, underscores the industry’s dynamic evolution. Additionally, creative payer-provider arrangements, or “payvider” models, will continue to evolve to provide more integrated and coordinated care to patients.
The pivotal element lies in aligning incentives to jointly meet consumer needs, essential for delivering comprehensive whole-person care and achieving improvements in market share and payer mix. Collaborative initiatives, exemplified by the partnership between Kaiser Permanente and Geisinger in launching Risant Health, further reflect an appetite and necessity for value creation for patients and sustainability. These initiatives emphasize the industry’s commitment to expanding access to value-based care.
A New Norm: The Dynamic Workforce™
Over the past two years, organizations have faced challenges in completing crucial projects due to staffing shortages amid the pandemic. The scarcity of resources has led many healthcare organizations to address this issue by hiring external contractors and consultants — what we call the Dynamic Workforce™.

RGP’s recent survey revealed that in 2022-23, 41% of healthcare organizations sought assistance from external project team members to supplement their workforce and ensure the completion of mission-critical projects, and it is projected to grow to 48%. The decision to bring in external talent is driven by various factors, including the desire to strengthen the current skills bench, introduce new perspectives, and critically evaluate new projects, along with the cross-pollination of ideas and the infusion of fresh perspectives into project initiatives.
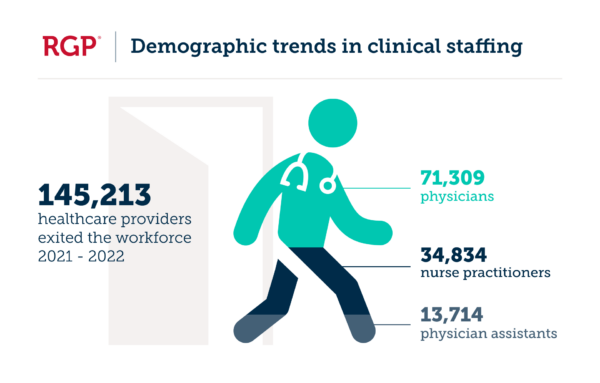
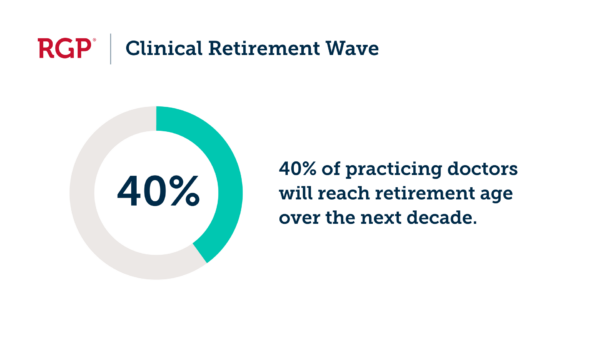
On the clinical side, from 2021 to 2022, approximately 145,213 healthcare providers exited the workforce, including 71,309 physicians, 34,834 nurse practitioners, and 13,714 physician assistants. Although some preliminary data at the end of 2023 suggested a slowdown in attrition, challenges persist. Research by the AAMC indicates that nearly 45% of practicing doctors are over 55, with more than 40% expected to be 65 or older in the next decade, posing risks of a significant retirement wave.
Staffing shortages and constant stress have led to increased medical errors, with 34% of doctors worldwide reporting such issues, according to SHG. This decline in patient volumes, exacerbated by staffing shortages, prompted health systems to rely on hybrid/dynamic labor, including travel nurses, to control costs amid financial losses.
Navigating Revenue Cycle Complexities and Outsourcing
The intricate healthcare reimbursement models, including Medicare, Medicaid, bundled payments and value-based care, underscore the urgency for operational efficiency. With the industry navigating complex landscapes and facing heightened financial pressures, we anticipate a surge in revenue cycle outsourcing to streamline operations and enhance revenue collection.
Against the backdrop of sustained financial pressure and the perpetual challenge for healthcare executives to do more with less, we will continue to witness an intensified focus on revenue cycle optimization and modernization. As healthcare organizations continue to grapple with consolidation in hospital operations and integration across entities, the emphasis on revenue cycle transformation becomes even more pivotal.
We anticipate a surge in revenue cycle outsourcing to streamline operations and enhance revenue collection.
This cross-functional perspective identifies new opportunities within and beyond revenue cycle management and necessitates the development of a comprehensive enterprise-wide strategy.
Due to misaligned incentives between payers and providers and the push for value-based care, revenue cycle outsourcing (especially in mid- and backend areas of the revenue cycle) will once again be among the top initiatives for healthcare executives navigating the complexities of 2024 and beyond.
Synergistic Future of Personalized Medicine and Generative AI
A dynamic interplay between two transformative forces—personalized medicine and generative AI is reshaping how providers approach patient care. This convergence represents a paradigm shift in healthcare, where treatments are not only based on individual genetic profiles but also dynamically optimized through real-time data analysis.
This powerful combination promises to revolutionize patient care, making precision treatment a standard rather than an exception.
Generative AI algorithms, fueled by extensive datasets, contribute to the identification of nuanced patterns and correlations within individual health records, enabling providers to make data-driven decisions in real-time. Fusing these advanced technologies amplifies the potential for personalized interventions, creating a healthcare ecosystem where every patient receives tailored treatments backed by the latest advancements in artificial intelligence.
However, challenges such as ensuring the ethical and responsible use of patient data, addressing privacy concerns and fostering widespread adoption across diverse healthcare settings may temporarily slow down the momentum, likely extending investment into the next year.
The Fusion of In-Person, Virtual and Hospital-at-Home Care
The landscape of healthcare delivery is set to undergo a transformative shift, breaking away from the traditional dichotomy of in-person versus virtual care. The emerging trend suggests that the majority of care delivery and patient interactions will evolve into an active hybrid model, seamlessly integrating both in-person and virtual elements. This holistic approach aims to provide a comprehensive healthcare experience that caters to the diverse needs and preferences of patients
The landscape of healthcare delivery is set to undergo a transformative shift, breaking away from the traditional dichotomy of in-person versus virtual care.
Anticipating this shift, we foresee continued investments and optimizations in virtual care, driven not only by technological advancements but also by the increasing emphasis on patient preferences and the proven efficacy of virtual care in delivering high-quality results. As the healthcare industry embraces this hybrid paradigm, it is poised to enhance accessibility, flexibility and overall patient satisfaction in the evolving landscape of healthcare delivery.
A key component of this evolution is the integration of hospital-at-home care, further expanding the boundaries of traditional healthcare settings and emphasizing the industry’s commitment to patient-centric, innovative care solutions.
Unveiling the Triad of Patient Engagement, Experience and Price Transparency
The acceleration of patient engagement, patient experience and price transparency is a pivotal trend for providers driven by the pressing need for a more patient-centric healthcare ecosystem. Healthcare providers recognize that engaged and empowered patients are more likely to proactively manage their health, leading to improved outcomes and reduced healthcare costs.
The increasing prevalence of chronic diseases and the shift towards preventive care underline the necessity for patients to play a more active role in their healthcare decisions. This trend aligns with the broader societal shift towards personalized and on-demand experiences, prompting healthcare providers to leverage technology to enhance patient engagement.
Access to healthcare services, reducing wait times and providing seamless communication between patients and providers will remain the key focus.
Additionally, the call for price transparency arises from the growing consumer demand for clarity in healthcare costs, enabling patients to make informed choices and fostering a more competitive and equitable healthcare market.
The convergence of these factors underscores why patient engagement, patient experience and price transparency are still categorized as top trends demanding a strategic response to the evolving expectations and needs of today’s healthcare consumers.
Continued Investments in Data and Analytics, Generative AI, Interoperability and Automation
Data and Analytics
The healthcare sector’s quest for enhanced decision-making, risk management and targeted interventions will continue to drive providers to invest significantly in advanced data and analytics tools. These investments will further empower healthcare organizations to derive meaningful insights from vast datasets, fostering evidence-based practices and ultimately improving the quality of care.
Generative AI
As artificial intelligence continues to redefine possibilities, Generative AI will emerge as a game-changer for healthcare providers, especially in administrative workflows such as automating routine tasks, reducing manual errors and unlocking operational efficiencies.
Additionally, Generative AI presents a range of transformative applications for healthcare providers, such as medical imaging analysis by enhancing image quality, segmenting and accurately identifying anomalies. Generative models can streamline electronic health record management through data summarization and automated clinical note generation.
AI-powered virtual assistants can be used for symptom assessment and remote monitoring. These collectively contribute to improved patient care, streamlined processes and advancements in medical research and treatment.
Interoperability
The seamless exchange of data across diverse healthcare entities is a cornerstone for coordinated care, enhanced patient outcomes and the industry’s shift towards collaborative healthcare ecosystems. Providers will continue to actively invest in interoperability solutions to break down data silos, fostering a connected healthcare environment that transcends traditional boundaries.
Automation
Automation is already proving to be a catalyst for operational excellence in healthcare. Providers are increasingly leveraging automation technologies to streamline workflows, reduce administrative burdens, and enhance the overall patient experience.
From optimized prior authorization workflows to enhanced care navigation, automation is reshaping healthcare delivery by ensuring efficiency and accuracy. We anticipate this trend to continue to permeate and experience increased adoption among providers.
Leading from the Forefront of Healthcare Innovation
In conclusion, the healthcare landscape is undergoing significant transformation driven by a combination of technological advancements, strategic consolidations, and evolving care delivery models. Therefore, providers must remain agile and forward-thinking to navigate these changes successfully.
By embracing trends such as personalized medicine, generative AI, Dynamic Workforce models, and a hybrid approach to care delivery, healthcare organizations can position themselves at the forefront of innovation, ensuring sustainability and enhanced patient outcomes in an increasingly complex and competitive environment.
